E 6 Oxygen Therapy
This equipment is mainly important for breathing problems as in
Breathing problems of a neonate and young infants. When oxygen is needed and how to deliver oxygen as well as when to stop it,
is described in
How to deliver Oxygen to a NYI.
Subsection of this chapter:
- Clinical Problem
- Assessment
- Management
- Infection Prevention
- Complications
- Care & Maintenance
- Troubleshooting & Repair
NEST360°. Newborn Essential Solutions and Technologies-Education – Clinical Modules: Oxygen
Therapy. (June 2020). License: CC BY-NC-SA 4.0.
Clinical Problem
Oxygen sources may be used to provide supplemental oxygen directly to patients,
shared between patients by using a flow splitter or used with other treatment
devices such as continuous positive airway pressure devices.
Supplemental oxygen is indicated for sick children, especially those with hypoxia. Hypoxia
is defined as an oxygen saturation (SpO2) < 90%.
See how to deliver oxygen for more information.
- Respiratory distress syndrome
- Transient tachypnoea of the newborn
- Birth asphyxia
- Meconium aspiration
- Pneumonia
- Pneumothorax
- Partial airway obstruction
- Neonatal anaemia
- Neonatal sepsis with respiratory distress
- Congenital anomalies (e.g., some types of congenital heart disease, diaphragmatic
hernia)
- Persistent pulmonary hypertension of the newborn
- Seizures
- Chronic lung disease
Whilst nearly all sick infants may benefit from oxygen therapy, any concentration of
oxygen administered without appropriate monitoring of
peripheral blood oxygen saturation
can cause harm.1 Carefully select between those that would benefit from
oxygen delivered directly to a patient (e.g., via nasal prongs) and those that would benefit
from supplemental oxygen delivered with pressure via CPAP. Monitor carefully and
discontinue oxygen as soon as it becomes unnecessary.
Assessment
Hypoxia contributes to both morbidity and mortality. Oxygen therapy may be used
to improve body tissue oxygenation, measured by SpO2 levels and also to provide
symptomatic relief.
Oxygen therapy may be delivered using oxygen concentrators
, oxygen flow splitters,
walled oxygen, and oxygen cylinders. Oxygen flow rates vary based on intended use and
mode of delivery:
- Resuscitation with bag and mask ventilation: 10 L/min1
(Alert 2.1)
- Flowmeter stand (Splitter): 1 – 2 L/min per oxygen port
- Prongs: up to 2 L/min
- Mask: from 3 L/min to 10 L/min
- CPAP: from 1 L/min to 6 L/min
| ! |
ALERT 2.1 |
| American Academy of Pediatrics resuscitation recommendations are 10
L/min of air, 21% Fraction of inspired oxygen (FiO2) for term babies and
30% FiO 2 for preterm babies.1 FiO2 should then be titrated with a blender
based on minutes of life and target SpO2 levels, which may not reach
85-95% until after 5-10 minutes of life. All sick newborns who are not
rapidly improving will need supplementary oxygen at increased FiO2. In
settings where blenders are not available FiO2 will not be able to be as
tightly controlled when oxygen is required during resuscitation.
|
Neonatal patients should reach SpO2 levels of 90 – 95% (Alert 2.1) by 15 minutes after
birth. (Alert 2.2) If oxygen is needed it is recommended to give between 0.5-1 L/min.2
Whilst on oxygen, regular monitoring should be conducted using a pulse oximeter to
ensure that this saturation range is maintained for the duration of treatment. Ideally,
patients suffering from severe respiratory distress should have continuous pulse oximetry
monitoring throughout care.2

| ? |
ALERT 2.2: SpO2 & Safe Oxygen Delivery |
When making this recommendation the following resources were
considered:
- According to the Textbook of Neonatal Resuscitation (NRP), 7th
Ed., “After birth, the oxygen saturation gradually increases above
90%. However, even healthy term newborns may take 10 minutes
or longer to reach this saturation” (p.77).1
- Target peripheral oxygen concentrations (SpO2) for newborns vary
depending on age and clinical condition. However, most authorities
agree that saturations between 90-95% minimises the
complications associated with both low and high oxygen levels
including death, neurodevelopmental impairment and Retinopathy
of Prematurity.3-6
|
Management
Management of oxygen therapy covers how to use the device in a variety of
settings, including patient preparation & commencement, care whilst on oxygen
therapy & removal of the patient from the therapy. See the modules on
oxygen concentrators
, oxygen cylinders and oxygen flow splitters,
for device specific recommendations.
PREPARING A PATIENT
- Assess the condition of the baby. Ensure all clinical management measures are
taken of which oxygen delivery is only one. Check the ABC and assess:
- Airway: suction if secretions are present
- Breathing:
- Respiratory rate: is it >60b/min
- SpO2: peripheral blood oxygen saturation level, is it <90%
- Work of breathing: e.g., grunting, fast breathing, chest indrawing
Chest auscultation
- Circulation:
- Perfusion: cool limbs and prolonged capillary refill time (>3 sec)
- Heart sounds
- Seizures
- Temperature
- If CPAP is available assess whether the patient would benefit more from bubble
CPAP than from oxygen alone. If so, prepare the patient for bubble CPAP.
STARTING A PATIENT
- Collect:
- Appropriately sized nasal prongs (should fit loosely in the nostrils)
- Tape
- Cotton wool
- Check that the end of the prong tubing is secured to the oxygen port on the
concentrator, flow has been set and that oxygen is coming out of the nasal prongs.
- Insert the nasal prongs and secure in place on both cheeks with tape. Adjust loop
adjustment slider to hold nasal prongs looped above the ears in place securely.
Protect the sides of the nose and cheek where the tubing could rub and injure the
skin. (3.1)
- Consider labelling nasal prongs to more easily determine which patients are being
treated with which oxygen ports. This will make it easier for future staff to adjust
oxygen levels & prevent incorrect changes from being made to the patient’s
treatment due to port misidentification. (3.2)


CARING FOR A PATIENT
- After starting on oxygen, monitor saturations using continuous
pulse oximetry.
Titrate oxygen up and down until normal saturation limits (SpO2 90 – 95)3–6 are
reached. If patient requires more than 2 L/min of oxygen, nasal prongs should be
changed to either CPAP or facemask (3.7) oxygen depending on the underlying
clinical condition. (Alert 3.2)
- Monitor according to clinical condition, or in accordance to local policy:
- Vital signs, including oxygen saturation, respiratory rate, heart rate, blood pressure
and temperature
- Work of breathing (see above)
- Nostril patency
- Administer nasal saline drops to prevent mucosal drying, every four hours or more
frequently depending on need.

| ? |
ALERT 3.2 |
Guidance on when to administer low flow oxygen versus bCPAP in
neonates is a complex decision which should be made on an individualised
basis for each country implementing comprehensive neonatal units with
bCPAP. It is a decision which must account for potential harms, benefits,
staff training, staff to patient ratio, infrastructure and allocation of care
within the health system.
NEST is aimed at implementing comprehensive neonatal care units with
bCPAP in low resource settings in order to reduce facility-based mortality
by 50% while also minimising morbidity. In light of potential harms
associated with hyperoxia, high burden of premature and low birthweight
infants in these types of units, and high patient to nurse ratios, 2L/min on
nasal cannula was felt to be a reasonable level at which to consider moving
a patient to bCPAP. This decision depends also on their clinical condition
and is consistent with WHO recommendations for “standard flow rates” for
neonates. At 2L/min from an oxygen cylinder, a 2kg infant may be receiving
close to 100% FiO27 and smaller infants may additionally be receiving
some amount of positive pressure2,7-9 which could be better regulated by
CPAP than by a low flow oxygen device.
|
REMOVING A PATIENT
- Once patients can maintain normal oxygen saturations and are clinically stable,
the oxygen flow rate should be reduced based on clinical response:
- Reduce oxygen flow by 0.25 L/min, rechecking saturations and clinical condition
after 15 minutes.
- If saturations and clinical condition remain stable, continue reducing oxygen flow
by increments of 0.25 L/min, rechecking saturations 15 minutes after each
reduction and then every 4 hours or as clinically indicated.
- If saturations drop below 90% or the patient clinically deteriorates, increase the
oxygen until normal saturations are obtained and the patient clinically improves.
- Once saturations are consistently above 90 - 95% at 0.25 L/min and the patient is
clinically stable, remove patient from oxygen by gently removing the tape and
taking the prongs out of the patient’s nostrils. Recheck the saturations after 15
minutes:
- If saturations have dropped or there is a clinical deterioration, recommence
oxygen.
- If saturations and clinical condition are stable, remove patient from oxygen.
Infection Prevention
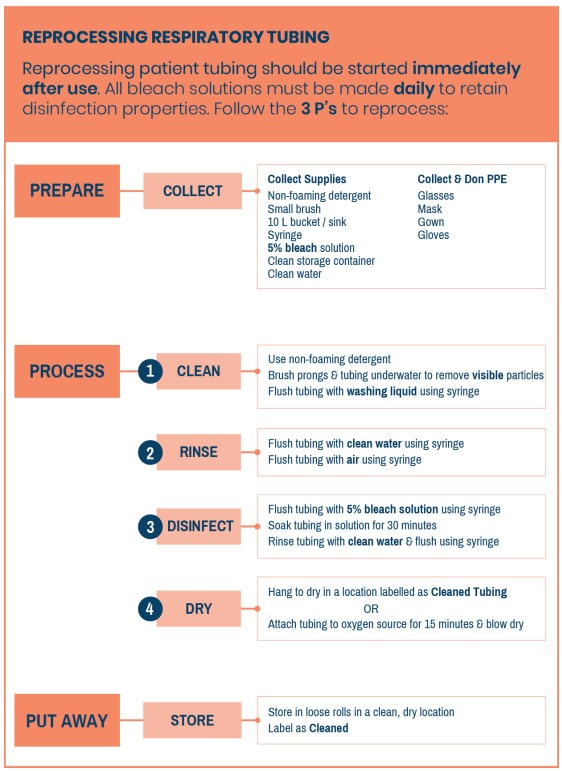
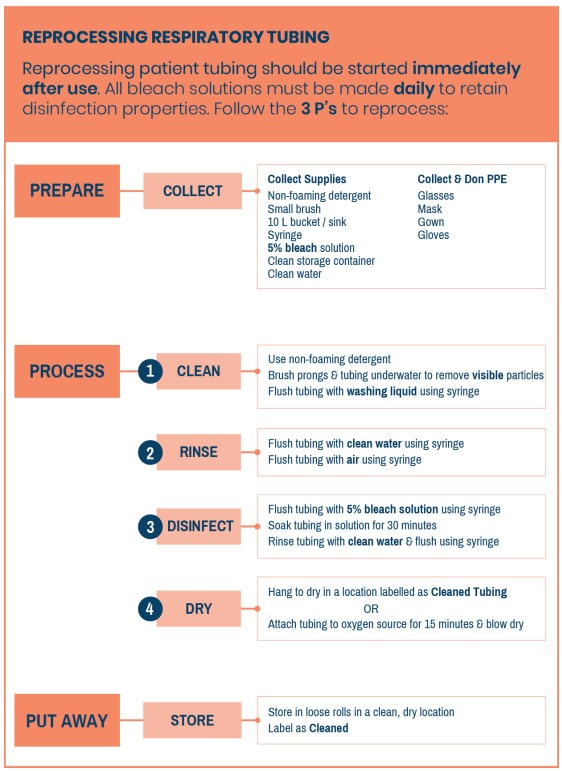
Routine and adequate cleaning of medical devices is critical to prevent hospital-acquired infections in newborn care units. If devices and equipment are not disinfected or reprocessed promptly or adequately between patients, they may pose a significant infection risk.
GENERAL INFECTION PREVENTION
- Clean hands with soap and water or alcohol before and after placing a patient on
oxygen or handling any tubing that will be used on a patient.
- Ensure that all patient-related tubing and consumables (including prongs and
humidifier bottles) are new or have been cleaned thoroughly before use. Any
patient-related tubing must be cleaned before it is used to place another patient on
oxygen. The Reprocessing Respiratory Tubing Algorithm details reprocessing
tubing for reuse.
- Tubing should be hung to dry after disinfection and should not touch the floor or
other unsanitary surfaces whilst drying. (4.2) It should be clearly labelled as having
been cleaned.
- All patient-related cleaned and new consumables should be stored in a clean, dry
location. Tubing should be stored in loose rolls, preventing sharp bends or kinks
which will decrease the lifetime of the tubing.

DISINFECTION AFTER USE
- Remove end of prong tubing from oxygen port. If reusing, immediately begin
hospital protocol for disinfection of tubing. Delay in initiating cleaning of reused
medical devices can lead to the need for more intensive cleaning procedures to
remove pathogens. If not reusing, discard appropriately. (Alert 4.1)
- If using a humidifier in the oxygen circuit, change water after each patient or daily,
if being used on the same patient.2
| ! |
ALERT 4.1 Reprocessing Single Use Devices
|
| Respiratory circuits and humidifiers associated with oxygen delivery are
generally intended as single use devices. However, in areas with limited
resources or challenging supply chains, this equipment is often re-used.
When re-processing single use devices it is extremely important that the
cleaning process is not delayed following completion of use. There
should be a detailed standard of practice as well as oversight processes
for ensuring timely and high-quality re-processing. If equipment is not
re-processed promptly or adequately between patients, it poses a
significant infection risk. Please refer to the Reference Manual for Health
Care Facilities with Limited Resources Infection Prevention and Control,
Module 610 for more detailed guidance on the re-processing of single
use devices.
|
REPROCESSING TUBING
Zoom in to see details
Complications
Introduction of equipment in newborn care units poses clinical and device
complications for patients. Awareness of potential complications is critical to
maximise patient safety.
CLINICAL COMPLICATIONS
- Hypoxia: if the nasal prongs become dislodged or blocked, the oxygen concentrator
malfunctions or is turned off there is a risk that the baby will not receive enough oxygen.
Hypoxia can cause:
- Damage to the brain (e.g. periventricular leukomalacia – damage to the white
matter of the brain)
- Multi-organ failure
- Death
Reference Alert 2.2 for a full discussion of oxygen saturation level targets and
recommendations.
- Hyperoxia: if the peripheral blood oxygen saturations (SpO2) are not monitored
appropriately or the flow rate is inadvertently changed there is a risk that the baby will
receive too much oxygen. Whilst oxygen can be lifesaving, peripheral blood oxygen
saturations (SpO2) above 95% on oxygen therapy can cause morbidities in premature
babies, including:
- Retinopathy of prematurity: in premature babies, high blood oxygen levels can
result in development of abnormal blood vessels on the retina, causing potential
visual impairment or even blindness.
- Chronic lung disease: prolonged use (although sometimes unavoidable) of oxygen
in premature babies causes lung fibrosis through inflammatory processes.
- Nasal blockage: the nasal prongs and nostrils can become blocked with mucus which
may result in increased respiratory distress and hypoxia.
- Necrotic septum: incorrectly sized or applied nasal prongs may result in pressure on the
nasal septum with resultant necrosis (tissue breakdown). Nasal septum should be
checked twice daily.
- Nasal prongs: prongs may become displaced, critically affecting the amount of oxygen
received by the patient. All health workers, including the parents/guardians involved in the
infant’s care should be aware of and watch out for this.
DEVICE COMPLICATIONS
Inadequate oxygen concentrations: all forms of delivered oxygen therapy are subject to issues
with oxygen concentration. This may result in inadequate levels of oxygen to treat respiratory
distress directly or through another device (e.g., CPAP).
Care & Maintenance
Power source, location and preventive maintenance will vary by oxygen therapy
type. See the modules on
oxygen concentrators
, oxygen cylinders and
oxygen flow splitters
for device specific recommendations relating to power source, ward
location and pertinent user preventive maintenance.
Troubleshooting & Repair
Typical failures and repair mechanisms will vary by oxygen therapy type.
See the modules on
oxygen concentrators
, oxygen cylinders and
oxygen flow splitters
for device specific recommendations.
References
Textbook of Neonatal Resuscitation (NRP), 7th Ed. (American Academy of Pediatrics,
2016).
Oxygen therapy for children. (World Health Organization, 2016).
Bancalari, E. & Claure, N. Oxygenation Targets and Outcomes in Premature Infants.
JAMA 309, 2161 (2013).
Cummings, J. J., Polin, R. A. & Committee on Fetus and Newborn. Oxygen Targeting in
Extremely Low Birth Weight Infants. Pediatrics 138, e20161576 (2016).
Manja, V., Lakshminrusimha, S. & Cook, D. J. Oxygen Saturation Target Range for
Extremely Preterm Infants: A Systematic Review and Meta-analysis. JAMA Pediatrics
169, 332 (2015).
Polin, R. A. & Bateman, D. Oxygen-Saturation Targets in Preterm Infants. New England
Journal of Medicine 368, 2141–2142 (2013).
Walsh, M. Oxygen Delivery Through Nasal Cannulae to Preterm Infants: Can Practice
Be Improved? Pediatrics 116, 857–861 (2005).
Locke, R. G., Wolfson, M. R., Shaffer, T. H., Rubenstein, S. D. & Greenspan, J. S.
Inadvertent administration of positive end-distending pressure during nasal cannula flow.
Pediatrics 91, 135–138 (1993).
Sreenan, C., Lemke, R. P., Hudson-Mason, A. & Osiovich, H. High-Flow Nasal Cannulae
in the Management of Apnea of Prematurity: A Comparison With Conventional Nasal
Continuous Positive Airway Pressure. Pediatrics 107, 1081–1083 (2001).
Curless MS, Ruparelia CS, Thompson E, and Trexler PA, eds. 2018. Infection Prevention
and Control: Reference Manual for Health Care Facilities with Limited Resources.
Jhpiego: Baltimore, MD.
World Health Organization. Technical specifications for oxygen concentrators. (World
Health Organization, 2016).